Baptist Medical Group-Memphis Primary Care was one of 11 primary care practices in the nation recognized in a Stanford University study for delivering high-quality care at a low cost.
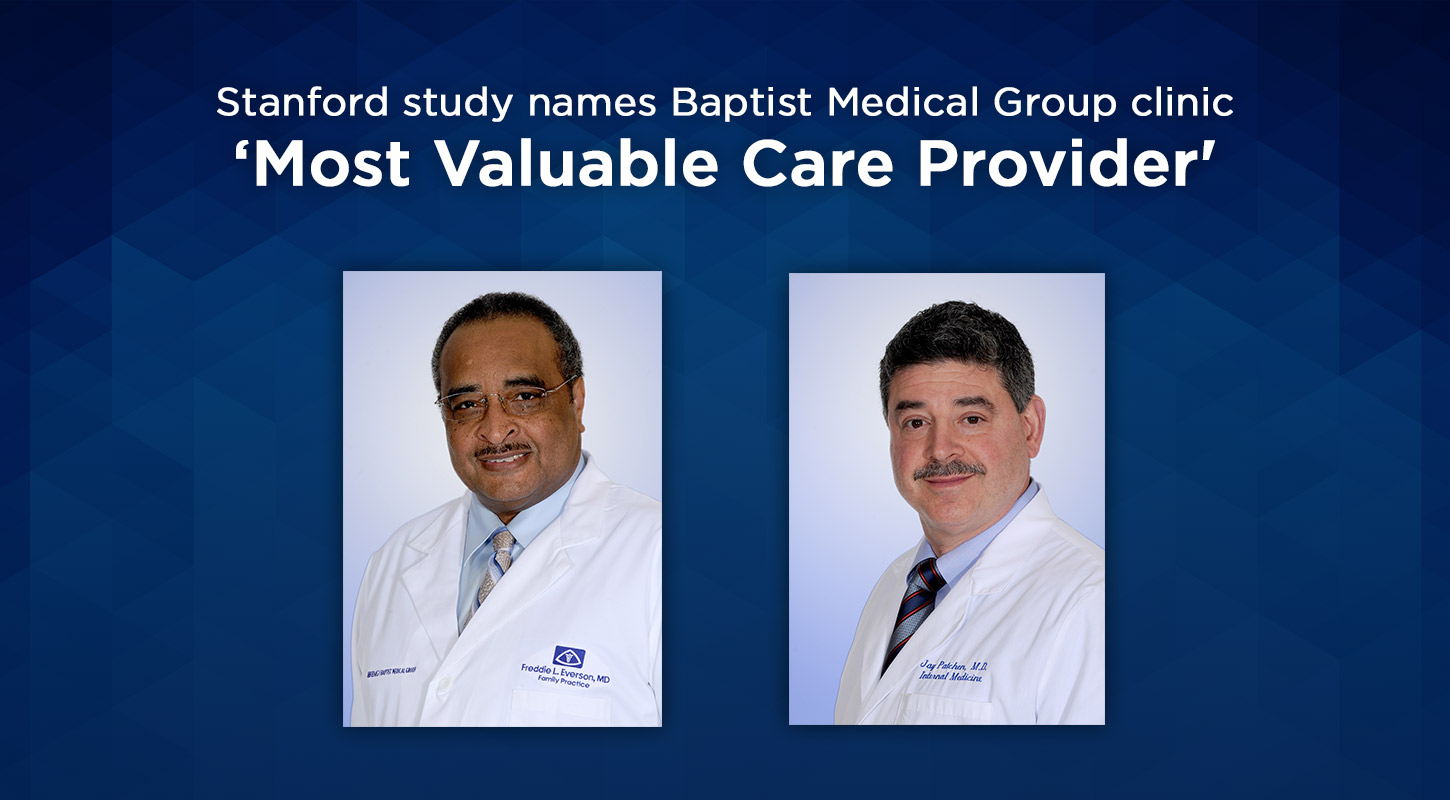
Researchers studied 15,000 primary care practices and identified 11 that deliver high-quality care at much lower-than-average total cost. One of those clinics was Baptist Medical Group-Memphis Primary Care, where Drs. Freddie Everson and Jay Patchen practice. Researchers found:
- The practice is noted for seeking and responding to feedback, and using it for improvement in the patient experience.
- Staff systematically ensure patients get recommended care, in or out of the practice, through careful follow-up.
- Physicians have a strong commitment to keep patients out of the hospital. They treat what they safely can in the office, take their own calls two out of three nights and give their cell phone number to patients they think are at risk of a health crisis.
“Our practice is committed to being responsive to patients, not only to their health, but to any concern or question that may arise,” said Everson. “We find that, if you take the time to listen to your patients and develop relationships with them, they are more apt to follow your advice, which leads to better health outcomes and less unnecessary testing. We always look at ways to improve our practice to better accommodate the patient’s needs.”
Stanford’s research team observed that the 11 high-performing primary care clinics differ in three ways from practices with average cost and quality scores:
- Their patient relationships were deeper
- Their interactions with the health care system were wider
- Their practice organization was team-based
The team identified 10 reasons why the clinics were able to establish and maintain deeper relationships with their patients.
- Practices are “always on.” The care team is always available, whether the practice is open or closed. Practices offer same-day appointments and accommodate walk-ins, extend evening and weekend hours, and more.
- Physicians follow quality guidelines and choose tests and treatments wisely. Physicians and staff ensure patients receive evidence-based care. At the same time, they conserve resources by tailoring care to the needs and values of their patients.
- They treat patient complaints as gold. Complaints from patients are regarded as valuable as compliments, if not more so.
- They in-source, rather than out-source, some needed tests and procedures. Primary care teams do as much as they can safely do—such as skin biopsies, insulin initiation and stabilization, joint injections or suturing— rather than referring patients elsewhere because the procedures take more time than the average patient visit.
- They stay close to their patients after referring them to specialists. Physicians refer to carefully chosen specialists whom they trust with their patients’ preferences and needs, and they stay in close communication as the specialists make care decisions.
- They close the loop with patients. The care team actively follows up to ensure that patients are seen rapidly after hospital discharges, are able to continue prescribed medications and see specialists when needed.
- They maximize the abilities of staff members. Physicians are supported by a team of nurse practitioners, physician assistants, nurses, and/or medical assistants. This enables physicians to spend more time with the patients who need the most direct physician contact, and to take care of more patients.
- They work in “hived workstations.” Care teams work in an open environment that facilitates continuous communication among both clinical and non-clinical staff.
- They balance compensation. Physicians are not paid solely on the basis of their productivity. Rather than basing physician income solely on service volume, pay typically also reflects performance on components like quality of care and patient experience.
- They invest in people, not space and equipment. By saving money on space, equipment and technology, these providers don’t need to see more patients or order expensive tests to generate a competitive income.
The primary goals of the study were to:
- Identify primary care practices that deliver higher quality at significantly lower total annual cost
- Determine the features that distinguish these primary care practices
- Create tools to enable other primary care physicians to incorporate insights from high-value providers into their own practices
- Demonstrate the replicable nature of these features and results, and support adoption on a national scale
For more information on the study, click here.
